Staphylococcus aureus in cats

Contents
About staphylococcus
staphylococcus — This is a genus of microorganisms, or rather bacteria belonging to the family Staphylococcaceae. “Staphylococcus” is translated from Greek as “bunch of grapes”. In stained smears under a microscope, these are round bacteria (cocci) that are arranged in groups and resemble bunches of grapes. Members of this family are widely distributed in nature. — they can inhabit the air, soil, water, and also live on the skin and mucous membranes of animals and humans.
Staphylococci are divided into two groups depending on the production of the enzyme coagulase: coagulase-positive and coagulase-negative. Coagulase-positive are the most pathogenic group and more often cause diseases (this includes Staphylococcus pseudointermediaus and Staphylococcus aureus). Coagulase-negative staphylococci can also cause disease.
For cats, the following types of staphylococci may be of importance: Staphylococcus pseudintermedius (staphylococcus pseudointermedius), Staphylococcus aureus (staphylococcus aureus), Staphylococcus schleiferi ssp (shuifer staphylococcus), Staphylococcus epidermidis (epidermal staphylococcus), Staphylococcus xylosus, Staphylococcus sciuri, Staphylococcus felis and others.
Staphylococcus pseudointermediaus is a commensal, that is, it can live on the body of an animal or a person without causing disease. It is not very common in cats. According to ongoing studies, from 6 to 22% of healthy cats are carriers of staphylococcus pseudointermedius. Already at an early age, staphylococcus aureus in kittens begins colonization in various parts of the body: for example, on the skin and mucous membranes. Colonization can take a lifetime. Only a small percentage of cats develop a clinical infection, this usually requires an underlying cause. — such as skin trauma.
Staphylococcus pseudointermediaus can lead to the development of opportunistic infections. Opportunistic infections — these are infections that do not cause disease in a healthy body, but can be dangerous if immunity is reduced.
aurococcus is not a commensal in humans and dogs. Staphylococcus aureus in cats is found in 20% of the population. Most often it is isolated from the skin and external auditory canals. The rather high prevalence of Staphylococcus aureus in healthy cats suggests that it may be a commensal. A number of studies have been conducted that have shown the presence of the same strain of Staphylococcus aureus in dogs and their owners, which may indicate the possibility of interspecific transmission. These studies have not been conducted with cats.
Staphylococcus aureus and other types of coagulase-positive staphylococci are much less common in cats — to 2%.
Coagulase-negative staphylococci are commonly found in healthy dogs and cats, as they are in other mammalian species. The location of various staphylococci in cats can vary, with some occurring in a specific location, others — in many places of the body. Coagulase-negative staphylococcus in a cat or cat without signs of disease is very often isolated from the skin, from saliva and from the mucous membrane of the oral cavity and genital tract. The most common is staphylococcus felis, less commonly isolated hemolytic staphylococcus, staphylococcus epidermis, staphylococcus simulans, staphylococcus saprophyticus. Despite the widespread colonization, diseases with coagulase-negative staphylococci are very rare.
Methicillin-resistant staphylococci. Methicillin-resistant/resistant staphylococci (MRS) are resistant to all β-lactam antibiotics (penicillins, cephalosporins, carbapenems) by producing an altered penicillin-binding protein.
Methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-resistant Staphylococcus pseudointermediaus (MRSP) are becoming a serious problem in veterinary medicine. Some strains, especially MRSP strains, are currently resistant to almost all available treatment options, making the management of the clinical disease they are involved in much more difficult.
Colonization with methicillin-resistant staphylococcus pseudointermedius can reach 1,2%, but it is an opportunistic pathogen and colonization does not necessarily lead to disease.
Methicillin-resistant Staphylococcus aureus is now being given special attention as a zoonotic disease. — a disease that can be transmitted to humans. But no clinical study has confirmed that staphylococcal colonization in cats or dogs may be an important factor in the spread of MRSA in humans.
Can you get Staphylococcus aureus from a cat?
At the moment, there is not a single study that would prove that a cat can be the primary source of human infection with staphylococcal infection. In medicine, the main factors of human infection with staphylococcus, including Staphylococcus aureus, are considered to be a decrease in immunity: HIV, chemotherapy, the use of immunosuppressive drugs, as well as the presence of wounds, including surgical ones. Much attention in medicine is paid to staphylococcus as a hospital infection, i.e. an infection that can be obtained in a medical institution with poor-quality disinfection.

Causes of Staphylococcus aureus
Diseases caused by staphylococcus aureus in cats are always secondary to the primary cause. For example, a skin infection occurs as a result of an allergic reaction or infestation with parasites; urinary tract infection — against the background of urolithiasis; respiratory system infection — against the backdrop of a viral infection.

The potential for a microorganism to cause disease is called the virulence factor. The main virulence factor of staphylococcus aureus — it is the ability to colonize different parts of the body. Staphylococci persist in the body, waiting for the moment when they can cause disease — for example, when traumatizing tissues or reducing immunity.
Virulence factors also include the ability of staphylococci to secrete various enzymes and toxins (hemolysins, proteases, lipases, etc.). Enzymes and toxins violate the integrity of tissues, thereby contributing to the development of inflammation and helping staphylococci to use damaged body tissues for nutrition.
In some situations, staphylococci can cause fatal diseases by producing certain toxins. For example, food poisoning can occur due to the fact that staphylococcus aureus has synthesized an enterotoxin as a result of improper storage of food. The synthesis of enterotoxin is determined by the presence of a certain gene in staphylococcus. This gene was found in isolates of Staphylococcus aureus and Pseudointermedius. Diseases mediated by staphylococcal enterotoxins do not occur in cats and dogs, but there is no evidence to suggest that domestic animals are inherently resistant to staphylococcal enterotoxins. Staphylococcus aureus can secrete an exfoliative toxin that can cause skin burn syndrome and toxic shock syndrome. The same toxin can be found in Staphylococcus pseudointermedius.
Staphylococcus aureus in kittens
Staphylococcus in kittens, as well as in adult cats, can develop secondarily against the background of the underlying disease. If a mother cat is a carrier of certain staphylococci, then in the process of caring for kittens, she will pass them on to them. If the kittens are healthy, staph infection will not pose a danger to them. Birth trauma, viral infections, artificial, unbalanced feeding, parasitic infestations — all this will be the reason for the development of a staph infection in kittens.

Symptoms
Staphylococcus aureus in cats plays a major role in the development of opportunistic infections — from superficial pyoderma (skin bacterial inflammation) to deep systemic infections. Opportunistic infections are caused by microorganisms that cannot cause disease in a healthy animal, but are manifested by a decrease in immunity or secondary to an already existing disease or injury. Decreased immune status in a cat can occur with chronic viral infections (feline immunodeficiency virus (FIV), feline leukemia virus (FLV) or long-term use of immunosuppressive drugs.
Pseudointermedius staphylococcus in a cat or cat most often causes skin infections. Less commonly, it can cause surgical infections, septic arthritis, osteomyelitis, urinary tract infection, liver abscess, peritonitis, and eye infections. Infections can vary in severity — from light to heavy.
Staphylococcus aureus in cats may be indistinguishable from Staphylococcus pseudointermediaus in presentation and severity.
Staphylococcus aureus shelfer most often presents in cats with pyoderma (skin infection) and otitis externa. Less commonly, infections may occur in other locations: the genitourinary or respiratory systems. Primary infections with coagulase-negative staphylococci are extremely rare. Among the staphylococci of this group, Staphylococcus felis deserves attention. With a urinary tract infection, it is often found. Therefore, Staphylococcus felis may be the primary pathogen.
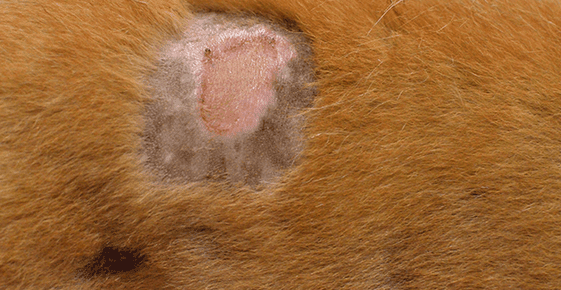
There are no specific clinical signs of staphylococcus infection in cats. Symptoms of the disease will be directly related to the damage to the organ or organ system. In skin diseases, these will be erosive or ulcerative skin lesions with loss of hair in the affected areas. With deep infections of the skin and subcutaneous tissue, abscesses will form. If the respiratory system is affected, we will see mucous, purulent discharge from the nose or cough. With inflammation of the urinary system, signs of cystitis will appear: frequent and painful urination, discoloration and transparency of urine. With a severe, deep and extensive infection, systemic non-specific signs will appear: refusal to eat, fever, lethargy.
I would like to separately note that bacterial, including staphylococcal, skin diseases in cats are always secondary to the underlying disease. This may be an allergic reaction or parasitic invasion, skin injuries received, for example, from other animals. At the same time, we can see signs of a concomitant disease — for example, flea feces from flea infestation.
Diagnostics
With staphylococcal infection, as already written earlier, there are no specific clinical signs. Cytological examination of stained smears may reveal the presence of septic inflammation.
But the final diagnosis is made only by bacteriological culture. — detection of bacteriological culture from the affected focus. The interpretation of the results obtained should be done with caution, especially when obtaining specimens collected from non-sterile sites such as the skin or respiratory tract. Considering that many staphylococci are initially commensals and can get into the collected material by accident, the material for bacteriological examination must be chosen carefully, to avoid contamination of the samples. One of the important aspects of bacteriological research — this is testing of the received samples for sensitivity to antibiotics. This is done in order to understand which antibiotics will suppress staph and which will be ineffective. This is especially important for methicillin-resistant strains.
Treatment of staphylococcus in cats
Treatment for staph in a cat will depend on the depth of the lesion, the amount of tissue affected, and the site of the infection.
The general treatment strategy is the same.
Systemic therapy is used to treat staphylococcus aureus in cats. — the use of antibiotics. Antibiotic therapy should ideally be selected based on bacteriological culture. Given the problem of the emergence of methicillin-resistant staphylococci, antibiotic therapy should be carried out under the supervision of a physician. Uncontrolled, misuse of antibiotics — insufficient dosage, small course, frequent use of different antibiotics — leads to the emergence of antibiotic-resistant strains of staphylococcus aureus in cats, dogs, other mammals and humans.
Local treatment makes it possible to cleanse damaged tissues of impurities and dead cells and deliver antibiotics and antiseptics directly to the site of infection. In the treatment of the skin, antibacterial shampoos, washes, lotions, creams and ointments are used. For arthritis — intraarticular injections. With otitis media — drops and lotions in the ears.

The ability to use an antibiotic directly in the focus of infection makes it possible to significantly increase its therapeutic concentration and, thereby, its effectiveness. Local treatment is of great importance for tissues where it is difficult to achieve the required concentration of the antibiotic through systemic use. A good example would be the treatment of otitis externa: the antibiotic is part of the ear drops and thus reaches the focus of inflammation, which is much more effective than systemic therapy.
It should be noted that during bacteriological examination and subtitration to antibiotics in the laboratory, standard dosages of antibiotics used in systemic therapy are used. By increasing the concentration of the antibiotic several times, it is possible to cause the death of staphylococci, which in laboratory studies have shown their resistance. Also, local treatment makes it possible to use antiseptics. — drugs that are not used for systemic therapy, such as chlorhexidine, povidone-iodine, benzoyl peroxide, silver sulfadiazine, mupirocin, etc. The use of these drugs is especially important when we are dealing with MRSA in a cat or cat when systemic therapy limited.
Sometimes surgery is needed to treat a staph infection. — for example, in the treatment of abscesses. During surgical treatment, necrotic tissues are removed, drains are installed to allow exudate outflow and access for the administration of antiseptics and ointments.

For deep and extensive infections, supportive treatment is required: infusion therapy, painkillers and antipyretics.
Prevention
Prevention is about maintaining the general health of the cat. To do this, follow these simple guidelines:
- High-quality and balanced nutrition;
- Carrying out preventive procedures: annual vaccination, regular treatment against endo- and ectoparasites;
- At the first signs of a cat’s discomfort (lethargy, cough, difficulty urinating, skin lesions), you should contact your veterinarian in a timely manner.
The article is not a call to action!
For a more detailed study of the problem, we recommend contacting a specialist.
Ask the vet
3 September 2020
Updated: 21 May 2022





