Blood transfusion for dogs
Hemotransfusion is the transfusion of sick animals with either whole blood, or components, or plasma protein preparations. This is a pretty serious procedure.In 80% of cases, blood transfusions in dogs are caused by anemia, and in 20% – by hemorrhagic shock. Blood transfusions sometimes save a dog’s life and play a decisive role in overcoming a critical condition.
Contents
- Purpose of blood transfusion in dogs
- Indications for blood transfusion in dogs
- Blood transfusion material for dogs
- Methods of administration
- Risks and Complications of Blood Transfusions in Dogs
- Blood transfusion to dogs as a method of treatment
- Who can become a donor
- Monitoring a dog’s condition during a blood transfusion
- Dog blood groups
Purpose of blood transfusion in dogs
- Substitution. Erythrocytes received from a donor remain in the recipient’s blood for 1-4 months, which increases the level of oxygen in the tissues.
- Stimulation – the impact on various systems and organs of the dog.
- Improvement in hemodynamics. Improving the work of the cardiovascular system, increasing the minute volume of the heart, etc.
- hemostatic target. Homeostasis is stimulated, moderate hyperoagulation is observed.
Indications for blood transfusion in dogs
- Identified acute bleeding, which is indicated by pale mucous membranes, weak and frequent pulse, cold paws.
- Chronic blood loss and unstable hemodynamics, indicating a lack of oxygen supply to the tissues in sufficient quantities.
- Non-recovering anemia of various etiologies.
- Hereditary or acquired coagulopathy, thrombocytopenia, leukopenia, hypoproteinemia.
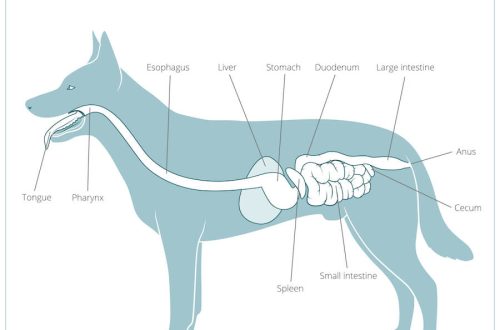
Blood transfusion material for dogs
The easiest way to obtain material from whole fresh blood. Therefore, it is widely used in veterinary medicine. Erythrocytes canned, stored chilled (temperature 3 – 60C) and used for 30 days or until the erythrocytes become discolored. Erythromass is necessary to replenish the reserve of erythrocytes (for chronic anemia) or at the risk of overloading with an additional volume of fluid. It is also used for acute blood loss (in combination with crystalloids). Plasma is necessary to restore clotting factors, incl. unstable components. The material is stored at -400C within 1 year. Before transfusion, it is heated to +30 – 370C, and then injected into the dog’s body as soon as possible.
Methods of administration
As a rule, blood and its components are administered intravenously. If it is impossible to inject blood into a vein (abscesses, severe edema), intraosseous infusion is used.
Risks and Complications of Blood Transfusions in Dogs
Acute complications are associated with a violation of the acid-base composition of the blood, errors in the transfusion technique, and hemodynamic disturbances. Delayed complications may be associated with transfusion of overheated, hemolyzed or infected blood: post-transfusion (hemolytic) shock, citrate (anaphylactic) shock, infectious diseases. Non-immunological reactions (acute form) manifest as fever. The reason is a reaction between an antigen and an antibody involving platelets, granulocytes or lymphocytes, or bacterial contamination of the blood. Sometimes there is an allergic reaction (urticaria with itching and rash). An increased load on the circulatory system is indicated by vomiting, tachycardia, irritability, cough, shortness of breath or cyanosis. Other risk factors:
- pulmonary edema
- transmissible infection
- fever
- post-transfusion circulatory overload
- hypervolemia
- acute post-transfusion reactions
- syndrome of multiple organ failure, etc.
The lungs, liver, endocrine glands and other systems and organs may be affected. Overloading can lead to acute dilation and cardiac arrest. Transfusion can cause an immunomodulatory effect and increase the risk of nosocomial infections, acute lung injury, autoimmune diseases. The most severe complication is anaphylactic shock. If even slight signs appear, the transfusion should be stopped as soon as possible.
Blood transfusion to dogs as a method of treatment
This procedure has become increasingly important in recent years. Its benefits have been repeatedly confirmed in the treatment of a number of hematological diseases. Due to the simplicity of the canine blood grouping system and the low levels of naturally occurring isoantibodies, veterinarians could almost ignore the incompatibility of blood types between the recipient and the donor. in a dog without damage to health (up to 10 ml / kg). The next blood sampling is carried out no earlier than in 45 – 60 days.
Who can become a donor
Once a dog can be transfused with blood of any group. But if a subsequent transfusion is required, the blood type must match. Rh-negative dogs can only receive Rh-negative blood. Any blood can be received by Rh-positive dogs. Sometimes an urgent blood transfusion is required. In this case, either a “random” donor is used (a healthy dog that ended up in the clinic for vaccination, nail trimming, etc.) or a pet of one of the doctors. The animal must be from 1,5 to 8 years old, it must be absolutely healthy .They take calm, docile dogs as donors. The body weight of the donor dog (muscle mass) must be more than 25 kg. The ideal blood type is DEA 1.1. negative. If the donor is a female, she must be nulliparous. The donor must not have left the local area.
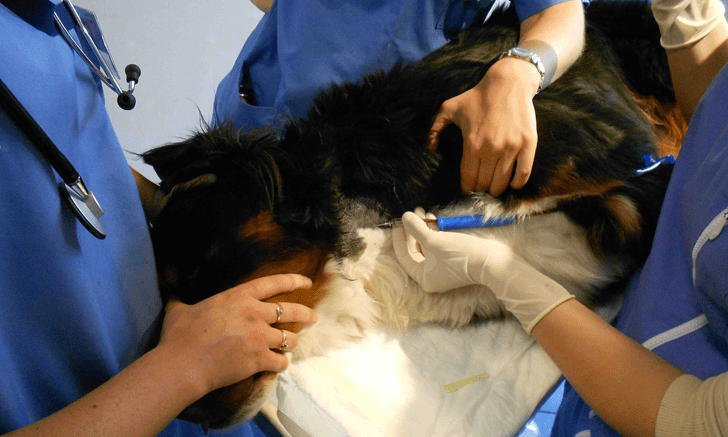
Monitoring a dog’s condition during a blood transfusion
Every 15-30 minutes during the transfusion and 1, 12, 24 hours after the procedure, the following parameters are evaluated:
- Behavior.
- The quality and intensity of the pulse.
- Rectal temperature.
- The nature and intensity of breathing.
- Color of urine and plasma.
- Mucosal color, capillary refill time.
- Prothrombin time and hematocrit are monitored before, immediately after completion, and 12 and 24 hours after the transfusion.

Dog blood groups
It is believed that dogs have 7 blood types. This is not entirely true. List A – G is a system of blood groups, or rather, only 1 of the options for the 1961 “release”. Since then, many more attempts have been made to streamline the data, and in 1976 developed the DEA nomenclature, which is now generally accepted in the United States. According to this nomenclature, blood systems can be designated as DEA 1.1, DEA 1.2, DEA 3, DEA 4, DEA 5, DEA 7 and DEA 8. The DEA 1 system is the most clinically relevant. This system has 3 gene-protein pairs and 4 possible phenotypes: DEA 1.1., 1.2, 1.3 and 0. One dog has only 1 phenotype. But dogs do not have antibodies to antigens of the other group, so a dog that has never had a blood transfusion before can be transfused with blood without DEA 1.1 compatibility, and the transfusion will be effective. But if a second transfusion is necessary, complications are possible. When DEA 1 is transfused into a negative recipient (phenotype 0) of the blood of a positive DEA 1 donor (any phenotype except 0), the recipient’s body after 7 to 10 days is able to produce antibodies to the DEA 1 antigen, which destroy any red blood cells, bearing this antigen. In the future, such a recipient will require only transfusions of DEA 1-negative blood, otherwise, instead of the standard 3 weeks, donor erythrocytes will live in the recipient’s body, at best, only a few hours, or even several minutes, which nullifies the effect of transfusion, and may even aggravate the situation. In this case, a positive DEA 1 donor can be transfused with the blood of a DEA 1-negative, however, with the condition that this donor has never been a recipient. The DEA 1 antigen is represented by a number of variants: DEA 1.1, DEA 1.2., DEA 1.3. blood DEA 1. the antibodies produced by it instantly destroy red blood cells with DEA 1.1. and cause an acute hemolytic reaction, fraught with severe complications. In this case, red blood cells with DEA 1.2 and 1.3 will agglutinate these antibodies, but not destroy them (although this is also bad for the patient). If we talk about the DEA 3 system, the dog can be either DEA 3 positive or negative. Transfusion of DEA 3 positive blood into an animal with appropriate antigroup antibodies (acquired or self) destroys the donor’s red blood cells and can cause acute transfusion reactions in the next 5 days. The DEA 4 system also has the + and – phenotypes. Without prior immunization, DEA 4-negative dogs do not have antibodies to DEA 4. Repeated transfusion of DEA 4-negative recipient, even in the presence of antibodies to DEA 4, does not cause a hemolytic reaction. However, a case of hemolysis is known in a dog that received incompatible blood transfusions several times in a row. The DEA 5 system is also positive and negative. 10% of DEA 5-negative animals have antibodies to DEA 5. Blood transfusion to a sensitized patient causes a hemolytic reaction and death of the donor’s erythrocytes within three days. The DEA 6 system has 2 phenotypes, + and -. Normally, there are no antibodies to this antigen. Blood transfusion to a sensitized recipient results in a moderate transfusion reaction and a moderate decrease in the lifespan of donor red blood cells. The DEA 7 system has 3 phenotypes: negative, 0, and Tr. Antibodies to Tr and 0 are present in 25% of DEA-negative animals, but they do not have a pronounced hemolytic effect. But with subsequent sensitization, others are developed that are able to decompose donor blood in less than 3 days. The DEA 8 system has not been properly studied. In addition to the above, there are other systems that are not included in DEA, since they were discovered recently, and a number of systems specific to certain breeds (for example, oriental dogs – Shibu-in, etc.) There are diagnostic kits for determining the absence or presence of DEA 1.1., 1.2, 3, 4, 5 and 7 antigens, but they are quite expensive. As a rule, in reality, especially in small towns, there are no ready-made donors, and compatibility is determined “on the glass”. However, this only eliminates the possibility of an immediate transfusion reaction, since the interaction of erythrocytes is monitored only until the drop dries, i.e.